What is HIV?
 HIV stands for Human Immunodeficiency Virus. It’s a virus that attacks the immune system, leaving people vulnerable to infections and cancers. The first cases of AIDS were reported in 1981. Today there are more than 35 million living with HIV/AIDS worldwide. In Canada, about 20,000 Canadians have been diagnosed as having HIV or AIDS. Today the use of antiretroviral drugs has reduced the spread of this virus tremendously.
HIV stands for Human Immunodeficiency Virus. It’s a virus that attacks the immune system, leaving people vulnerable to infections and cancers. The first cases of AIDS were reported in 1981. Today there are more than 35 million living with HIV/AIDS worldwide. In Canada, about 20,000 Canadians have been diagnosed as having HIV or AIDS. Today the use of antiretroviral drugs has reduced the spread of this virus tremendously.
How does it spread?
The most common way you can get infected with HIV is through sexual contact with an infected person. You may also be exposed if your blood comes into direct contact with someone who has the disease. If you share sex toys such as dildos, vibrators, anal beads, etc., they could potentially transmit HIV. Sharing razors or toothbrushes without sterilizing them after use increases your risk of infection.
HIV infection causes damage to many parts of the body including:
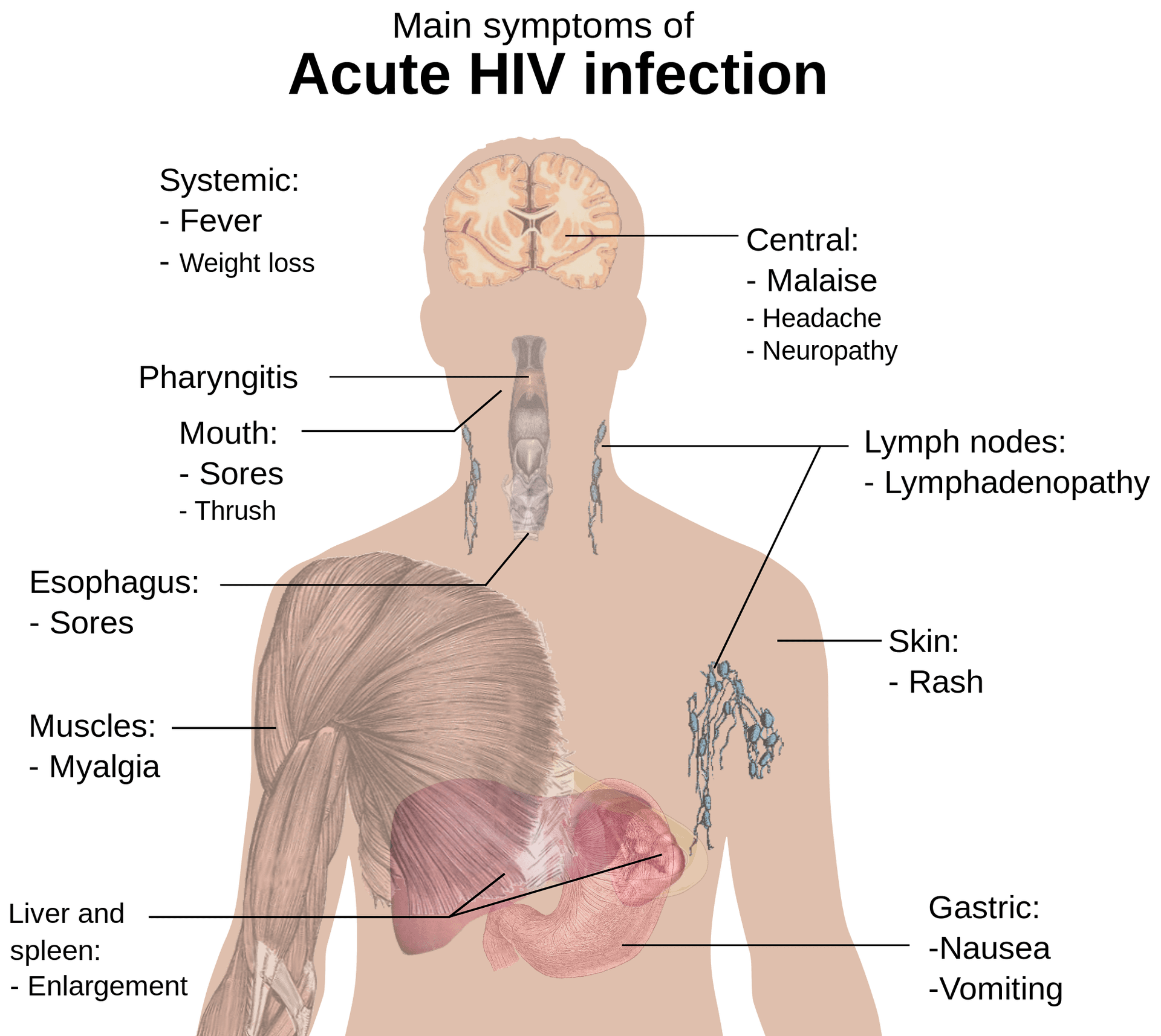
Immune system – CD4+ lymphocytes are white blood cells that help fight infections. The immune system becomes weaker during HIV infection because the number of CD4+ lymphocytes decreases. As more viruses enter the bloodstream, the immune system cannot keep up. Eventually, the immune system fails completely and patients become susceptible to life-threatening opportunistic infections such as pneumonia, tuberculosis, herpes simplex type 2, and others.
Digestive tract – People who live long enough develop chronic diarrhea which leads to malnutrition. Many people lose appetite and suffer weight loss. Others complain of stomach cramps, bloating, gas and constipation. Sometimes there is no obvious reason why someone develops AIDS-related digestive disorders.
Heart – Heart disease is common among those infected with HIV. There are several reasons for this. First, high levels of cholesterol and triglycerides increase the risk of a heart attack. Second, inflammation caused by HIV increases the risk of atherosclerosis. Third, certain types of cancer occur much more frequently in people living with HIV/AIDS. Finally, medications used to treat HIV itself can be toxic to the cardiovascular system.
Skin – Skin conditions associated with HIV include Kaposi sarcoma, oral candidiasis, thrush, shingles, molluscum contagiosum, warts, fungal nail infections, bacterial infections, scabies, ringworm, eczema, psoriasis, lichen planus, erythema multiforme, pemphigoid among others.
Antiretroviral Therapy
Antiretrovirals are the most important drugs in treating HIV infection. They work by blocking or slowing down the replication of a virus that causes AIDS, and they can be used alone to treat people with early-stage disease or combined with other medications for more advanced cases.
The first drug approved was AZT, which is still widely prescribed today. Other commonly used agents include:
Abacavir – A nucleoside reverse transcriptase inhibitor. It has been shown to reduce mortality rates among patients who have not yet developed full-blown AIDS.
Didanosine – An NRTI. Has been found effective against some strains of HIV. Used as part of combination therapy.
Efavirenz – Another NRTI. Effective at reducing viral load when given together with another agent such as ZDV.
Fluorouracil – Antimetabolite. Can cause bone marrow suppression. May also increase the risk of heart problems.
Indinavir – Protease Inhibitor. Blocks an enzyme needed for the production of new viruses from mature ones. Also blocks enzymes produced by bacteria that normally live on human skin. This may help prevent the transmission of HIV through sexual contact.
Lamivudine – Thymidine analog. Causes mitochondrial damage leading to liver failure if taken long term.
Nelfinavir – Proteasome inhibitor. Reduces levels of circulating immune cells called CD4+ T lymphocytes.
Saquinavir – Protease inhibitor. Prevents the cleavage of proteins necessary for the reproduction of the virus.
Stavudine – Nucleotide analog. Increases survival time but does not cure HIV/AIDS.
Tenofovir – Nucleotide analog. Highly active antiretroviral treatment regimen consisting of three different classes of medication.
Zidovudine – Nucleoside analogue. Decreases the amount of virus present in the bloodstream.
Combination therapies
In addition to single-drug treatments, combinations of two or more antiviral drugs are often used to slow the progression of HIV.
HIV Viral Life Cycle
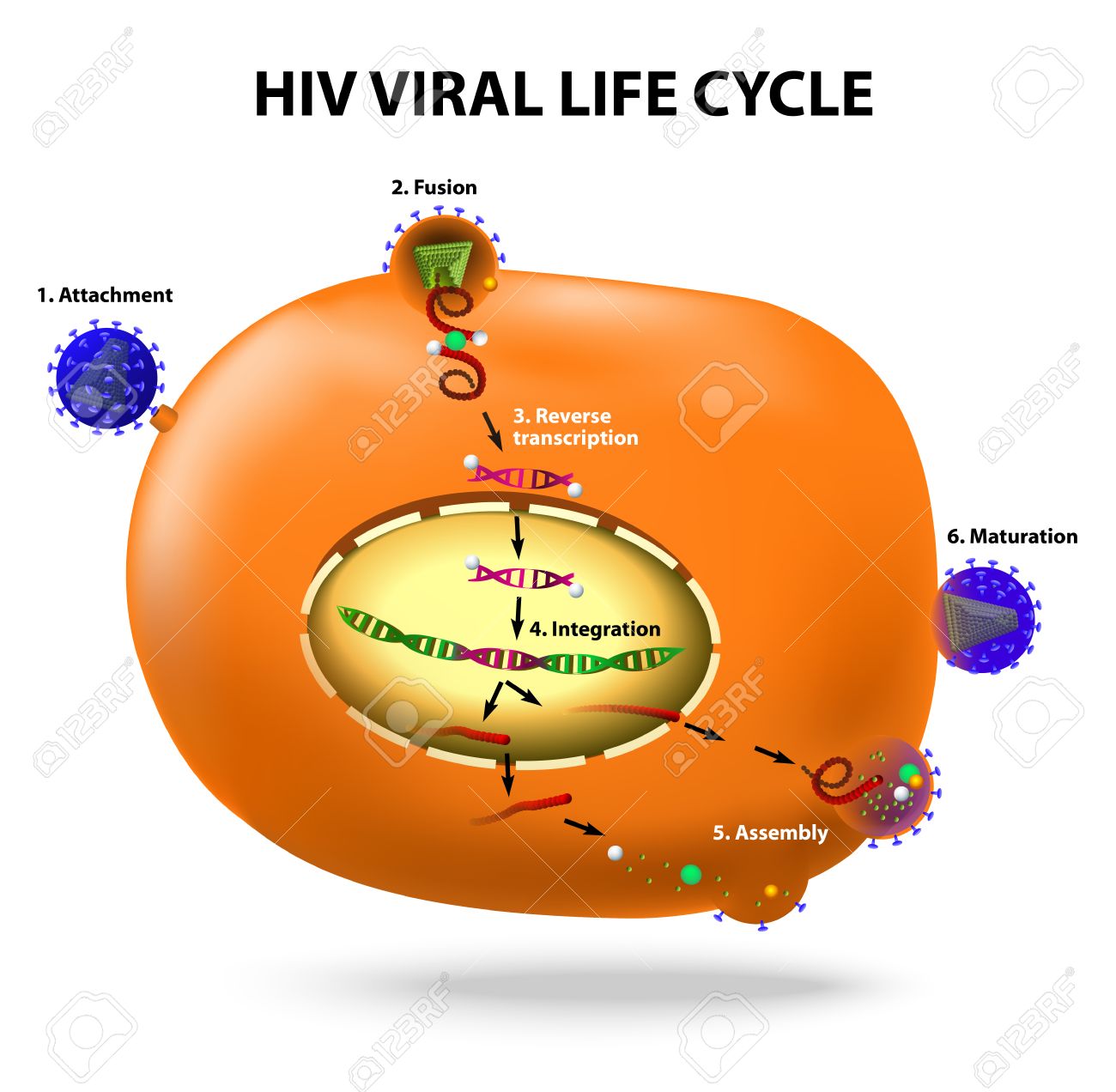
There are four stages of the life cycle of HIV. Each stage requires specific steps to occur before it proceeds into the next one. These steps are known as “virus entry”, “uncoating”, “reverse transcription” and “integration”.
Entry
When a person becomes infected with HIV, the virus enters their body via mucous membranes or breaks open small wounds. Once inside the cell, the virus attaches itself to receptors on the surface of the cell membrane. There are several types of these receptors; each type binds to a particular protein on the outside of the cell wall. Some of these receptor sites are located on white blood cells, while others are found on certain parts of the brain, lungs, kidneys, intestines, etc.
Uncoating
Once attached to its target site, the virus must uncoat so that it can enter the host’s cytoplasm. Uncoating occurs after attachment to the cellular receptor. During this process, the outer coat of the virus dissolves away, exposing the core structure of the virus. Inside the core, there are many copies of RNA surrounded by capsids made up of multiple layers of protein. The capsids contain genetic material which is then transcribed into DNA using reverse transcriptase. Reverse transcriptase converts the RNA copy of the genome into double-stranded DNA.
Reverse Transcription
The newly formed DNA now has all the information required to make additional copies of the virus. It uses ribonuclease H to remove any remaining pieces of RNA left over from the original infection. Ribonuclease H removes the last piece of RNA from the viral DNA strand. After the removal of the RNA, the DNA is ready to be integrated into the host chromosome.
Integration
The final step in the replication cycle involves inserting the viral DNA into the host chromosome. Integration takes place at random locations throughout the chromosomes. However, some regions have been shown to be preferred targets for integration. One such region is near the centromere.
This area contains genes important for the proper functioning of the cell. If integration happens here, the risk of developing cancer increases significantly. Other areas where integration may happen include telomeres, immunoglobulin gene clusters, TCR loci, proto-oncogenes, growth factor genes, and other regulatory sequences.
How Does Antiviral Therapy Work?
The goal of antiviral therapy is to keep the number of active viruses low enough so that the immune system can control them without causing damage to cells. The best way to achieve this balance is to suppress the number of actively infected CD4+ T lymphocytes below 200/mm3.
HIV Replication Cycle: How Do Anti Virals Affect That Process?
There are three main stages involved with replication of HIV – attachment, integration, and maturation. Each stage requires different steps to be completed successfully. When we say “antiviral agents inhibit HIV at each step of the cycle” what we really mean is that they prevent certain enzymes needed during those specific phases of the process from functioning correctly.
NRTIs
NRTIs inhibit reverse transcriptase. Nucleoside analogs like AZT work by binding directly to the active site of RT. This prevents the formation of an essential intermediate during the conversion of the viral RNA to DNA. As a result, no new viruses can form.
Non-Nucleosides
NNRTIs interfere with HIV replication through inhibition of reverse transcription. These inhibitors act as competitive substrates for the enzymes responsible for converting the single-stranded RNA genome into double-stranded DNA. By blocking one or more steps in the pathway leading to the formation of mature viral particles, they reduce the amount of virus produced within infected cells.
Protease Inhibitors
PIs target two different sites on the protease molecule that allow it to cleave itself out of the Gag/GagPol polyprotein precursor. PIs also interact with another part of the Gag/ProPol polyprotein called PR1. When this interaction occurs, the PR2 domain becomes exposed and allows the release of free ProPol. Free ProPol is able to assemble into immature virus particles.
The presence of these immature particles causes premature activation of the immune system. Once released, the immature particle matures inside the cytoplasm before being transported to the plasma membrane. At the plasma membrane, the immature particle fuses with the outer layer of the lipid bilayer surrounding the cell.
The resulting fusion process releases the contents of the envelope into the extracellular space. The newly formed capsid then travels along microtubules towards the nucleus. Inside the nucleus, the capsid uncoats and disassembles releasing the nucleic acid into the cytosol.
From there, the genetic material enters the ribosomal machinery which translates the information contained in the RNA into protein.
Other Classes of Antiretrovirals
The following classes are used less frequently than the above-mentioned ones but still play an important role in treatment regimens.
Entry Blockers
They prevent the entry of the virus into the cell. Maraviroc is currently under investigation. It targets the CCR5 receptor. Other compounds include TAK779, SCH 417690, AMD3100, etc.
Enzyme Inhibitors
This class includes ritonavir, saquinavir, and indinavir. Indinavir inhibits both the aspartyl protease and the helicase activity of HIV RT. Saquinavir inhibits only the aspartyl proteases. Ritonavir inhibits CYP450 3A4 and therefore reduces the metabolism of other medications. All three drugs have been shown to be effective when combined with at least one NNRTI. However, their effectiveness has waned due to the development of resistance mutations.
Integrase Strand Transfer Inhibitor
These agents inhibit the integration of the proviral DNA into host chromosomal DNA. This prevents production of new copies of the virus from integrated genomes. They do not affect the synthesis of viral proteins. INSTIs bind to the enzyme’s catalytic center and block the ability of the enzyme to perform its function. Raltegravir was approved by FDA in 2007. Elvitegravir was approved in 2011. Dolutegravir was approved for use in 2013.
It’s important that you feel ready to start ART and understand how to take it properly. Once you start ART it’s very important that you take it properly and don’t miss or skip doses, as this can lead to something called HIV drug resistance, and may mean that your drugs don’t work as well for you in the future.
What Is cART?
The acronym cART stands for “combination antiretroviral therapy.”
cART is a combination of three or more drugs that are used to treat HIV.
The most common combinations include:
– Atripla – This drug combo has been shown in clinical trials to be effective at reducing the amount of virus in your body by up to 99%. It also helps prevent resistance from developing against other anti-HIV medications.
– Complera (emtricitabine/rilpivirina) is indicated for the treatment of HIV infection in adults. It may be used alone or with other antiretroviral agents, including efavirenz and nevirapine. Complera has been shown to reduce plasma viral load by approximately 1 log10 copies per milliliter compared with placebo when administered once daily as a single dose at any time during the day.
– Truvada + emtricitabine + raltegravir: This triple combination works well when combined with another class of antiviral agents called integrase inhibitors. These work by blocking an enzyme needed to make new copies of the viral genome. Integrase inhibitors have fewer side effects than some previous treatments but they do not cure people who already have full-blown AIDS. They can, however, help keep the disease under control and reduce the risk of transmission.
– Stribild: Stribild combines two different classes of medicines — NS5A replication complex inhibitor and protease inhibitor. Both of these types of medicine target specific steps in the life cycle of the virus. In addition, it contains elbavirdin which targets the hepatitis C virus as well. –
– Triumeq: Triumeq consists of 3 pills taken once daily. Each pill includes 2 parts of dolutegravir plus 1 part of lamivudine. Dolutegravir blocks one step in the life cycle of HIV while lamivudine inhibits reverse transcriptase.
Does the antiretroviral treatment have side effects?
Antiretroviral therapy does not cause weight loss or hair thinning as chemotherapy would. It doesn’t affect fertility either. Some people report feeling tired when first starting treatment but most people get better over time.
Antiretroviral drugs can sometimes cause nausea, diarrhea, headaches, mouth sores, skin rashes, fatigue, muscle pain, dizziness, insomnia, mood changes, and problems sleeping through the night.
These symptoms usually go away after a few weeks on medication. If they persist longer than two months, talk to your doctor about changing your dose or stopping some of your medicines. You should also tell your healthcare provider if you experience any unusual bleeding or bruising while taking these medicines.
What Is HIV Drug Resistance?
Skipping doses or starting and stopping medication can lead to drug resistance, which can harm your health and limit your future treatment options.
Resistance occurs when mutations develop within the genome of viruses causing resistance to antiviral medications. This results in decreased susceptibility to one or more classes of medication. There are two types of drug-resistant viruses: primary and secondary.
Primary resistance develops after initial exposure to a particular class of medication; this type of resistance cannot be overcome by changing the regimen.
Secondary resistance arises because of mutation acquired during previous exposures to other medications. It usually requires changes in both the current and prior regimens.
In fact, there are several new classes of antiretrovirals available now that could potentially treat someone who has developed drug resistance.
HIV Therapy in Pregnancy
If you’re pregnant, you need to know what kind of care is best for you and your baby. Your pregnancy will likely require different kinds of tests and procedures than usual. The information below will help answer many questions you might have about HIV during pregnancy.
How Does HIV Affect My Baby During Pregnancy?
In addition, HIV affects the fetus before birth. When the mother becomes infected with HIV, her immune system begins attacking cells containing the virus. These cells include those lining the inside surface of the placenta, where blood flows between the maternal bloodstream and fetal circulation. As a result, the amount of oxygen delivered to the developing brain decreases. This causes damage to the central nervous system and results in low IQ scores among children born to mothers with untreated HIV.
The risk of transmission from mother to child increases throughout gestation. By the end of the third trimester, nearly 100% of babies exposed to HIV at birth develop AIDS within five years. However, only 10%-15% of infants whose mothers receive effective prenatal care and antiviral medications transmit the disease to their offspring.
Can Antiviral Drugs Be Used To Treat HIV Infection While Pregnant?
Yes! There are currently three FDA-approved antiretroviral regimens used to prevent vertical transmission of HIV. All three involve daily oral administration of either zidovudine, lamivudine, or tenofovir disoproxil fumarate. AZT was originally prescribed as part of triple therapy until it became clear that its use increased the rate of congenital abnormalities such as heart defects.
Is Treatment Necessary For A Healthy Mother And Child?
Even if you’ve been diagnosed with HIV while pregnant, you should continue taking your medication. You can also start on combination therapy right away after delivery. Studies show that women who begin treatment early in pregnancy experience fewer complications and lower rates of infant mortality compared to women who delay starting treatment until later in pregnancy.
When Should I Start Taking Medication After Delivery?
If you’re planning to breastfeed, you must take your meds immediately following delivery. Breastfeeding requires high levels of antibodies which protect newborns from infection. Without these proteins, the infant’s body would become vulnerable to viral infections like HIV. In fact, studies suggest that breastfeeding protects an infant from acquiring HIV even when the mother has no detectable level of the virus in her milk.
However, there is some evidence that suggests that certain drugs interfere with lactation. Therefore, before beginning any new drug regimen, talk to your doctor about whether this will affect your ability to nurse.
How Can My Partner Help Me Take Care Of Our Baby?
Your partner can help you take good care of yourself during pregnancy. He/she can provide emotional support and encouragement. Your partner can also assist you with household chores so that you have more time to focus on your health. It’s important that both partners work together to ensure that each person takes proper care of themselves. This way, neither one feels neglected.
Will my baby inherit HIV from me?
No. The risk of passing HIV onto a child via vaginal birth is extremely low. However, babies born to infected moms face other risks including premature labor, respiratory distress syndrome, jaundice, and death. Babies born vaginally to untreated mothers are at higher risk than those delivered by cesarean section. Cesareans carry their own set of risks including bleeding, wound healing problems, and scarring.
Can I Get Pregnant While On Antiretrovirals?
Yes! There are many different types of medications available today. Many of them allow you to conceive without having to stop taking your medicine. Talk to your healthcare provider about what type of regimens might best suit you.
Are There Any Side Effects From Combination Therapy?
Combination therapies for treating HIV include three or four antiretroviral agents taken simultaneously. These combinations may be used as initial treatments or maintenance therapies. They may also be prescribed to prevent transmission of HIV to infants through breastfeeding. Side effects vary depending upon the specific medications being combined.
What Are Other Options To Treat HIV Infection During Pregnancy?
There are several options besides combination therapy. Some women choose not to use medication because they want to avoid exposing their unborn children to potentially harmful substances. Others prefer natural remedies such as herbs and vitamins. Still, others opt for alternative methods such as acupuncture, massage, yoga, meditation, exercise, dieting, and stress reduction techniques. All of these approaches offer benefits but none offers complete protection against HIV.
Use of Antiretroviral Agents in Pediatric HIV Infection
The use of antiretroviral agents in children has been limited by concerns about toxicity and a lack of data on efficacy. However, recent studies have shown that these drugs are safe and well-tolerated when used appropriately. Furthermore, preliminary evidence suggests that they also improve clinical outcomes such as growth velocity and immune function. These findings support their continued use in pediatric patients who require them.
What is the cost of antiretroviral therapy?
Antiretroviral therapies are expensive.
The cost of antiretrovirals is a major barrier to the treatment and prevention of HIV infection in developing countries, where most people with AIDS live. The World Health Organization estimates that more than half of all patients who need antiretroviral therapy cannot afford it. In addition, many patients do not adhere to their medication regimens because they have no access to affordable medications or transportation to get them.
Some governments subsidize drugs only if they are purchased within certain limits. For example, in South Africa, government subsidies cover up to 80% of the costs of first-line ARV regimens when provided free of charge. But once the patient reaches this limit, he/she must pay out of pocket. If the patient does not reach this limit, then there will be no subsidy. Patients often end up paying much more than necessary due to a lack of insurance coverage.
In contrast, private health plans usually provide full coverage regardless of income level. They may be covered by insurance plans but they often come with co-payments. If you don’t qualify for coverage through Medicaid or Medicare, you’ll probably pay out of pocket. Some people choose not to get ART because they cannot afford them. Others decide against getting treatment because they believe that they do not need it.
How can we help reduce the cost of antiretroviral therapy?
We should work together to find ways to make sure everyone has access to life-saving medicines. We can start by working on policies that ensure universal access to quality care. This means ensuring that every person living with HIV receives comprehensive medical services, including antiretroviral treatment. It also includes providing support so that those without adequate resources can obtain needed healthcare.
For more reading: